Why Is Obesity Considered as One of the Trigger Factors for the Emergence of Diabetes?
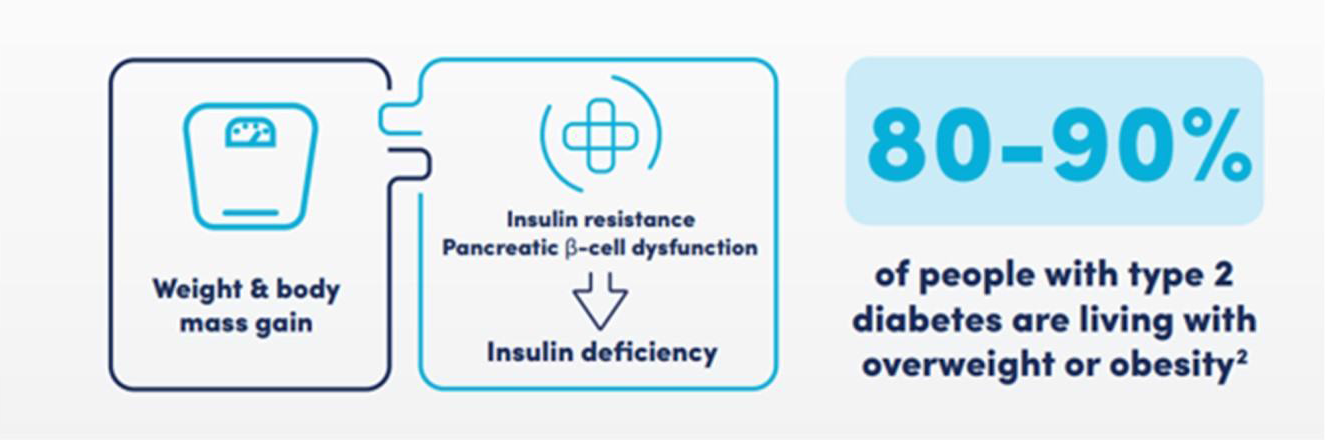
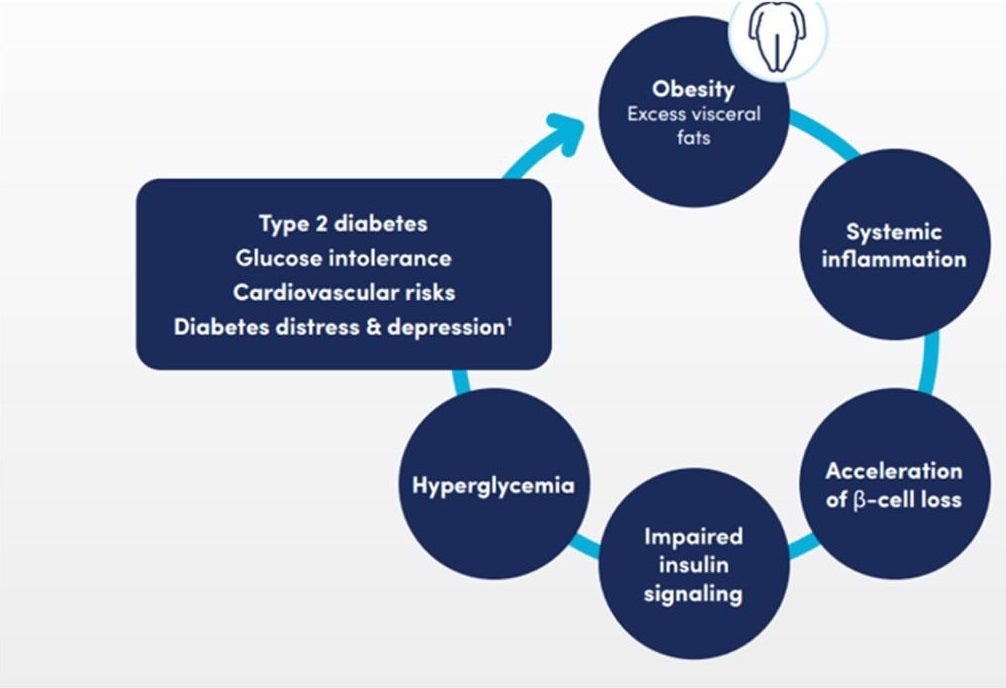
Obesity is at the heart of driving type 2 diabetes (T2D) pathogenesis because it is a driver of insulin resistance, pancreatic β-cell dysfunction, and systemic inflammation. 80-90% of people living with T2D have an overweight or obese body mass index (BMI). For these patients, visceral fat leads to disrupted glucose metabolism, insulin resistance, and cardiovascular risk.1 Evidence-based and early treatments targeting obesity are critical for attaining remission of diabetes.2 Figures 1 and 2 show the underlying critical role of obesity and visceral fat in the pathogenesis of T2D and its complications.1
Since obesity plays such a central role in triggering T2D, managing weight should be a priority in treatment. So, what are the most effective and sustainable weight loss dietary strategies?
Diabetes Diet for Weight Loss
The primary goal of treatment is achieving and maintaining weight loss. Diabetes diet meals such as Meal Replacement Products (MRPs) and Very Low-Calorie Diets (VLCDs) represent evidence-based treatments for weight loss in obesity.3,4 The inclusion of MRPs in a diabetes diet plan to lose weight allows for faster initial weight loss compared to other diet plans.5
Diabetes Nutrition Guidelines
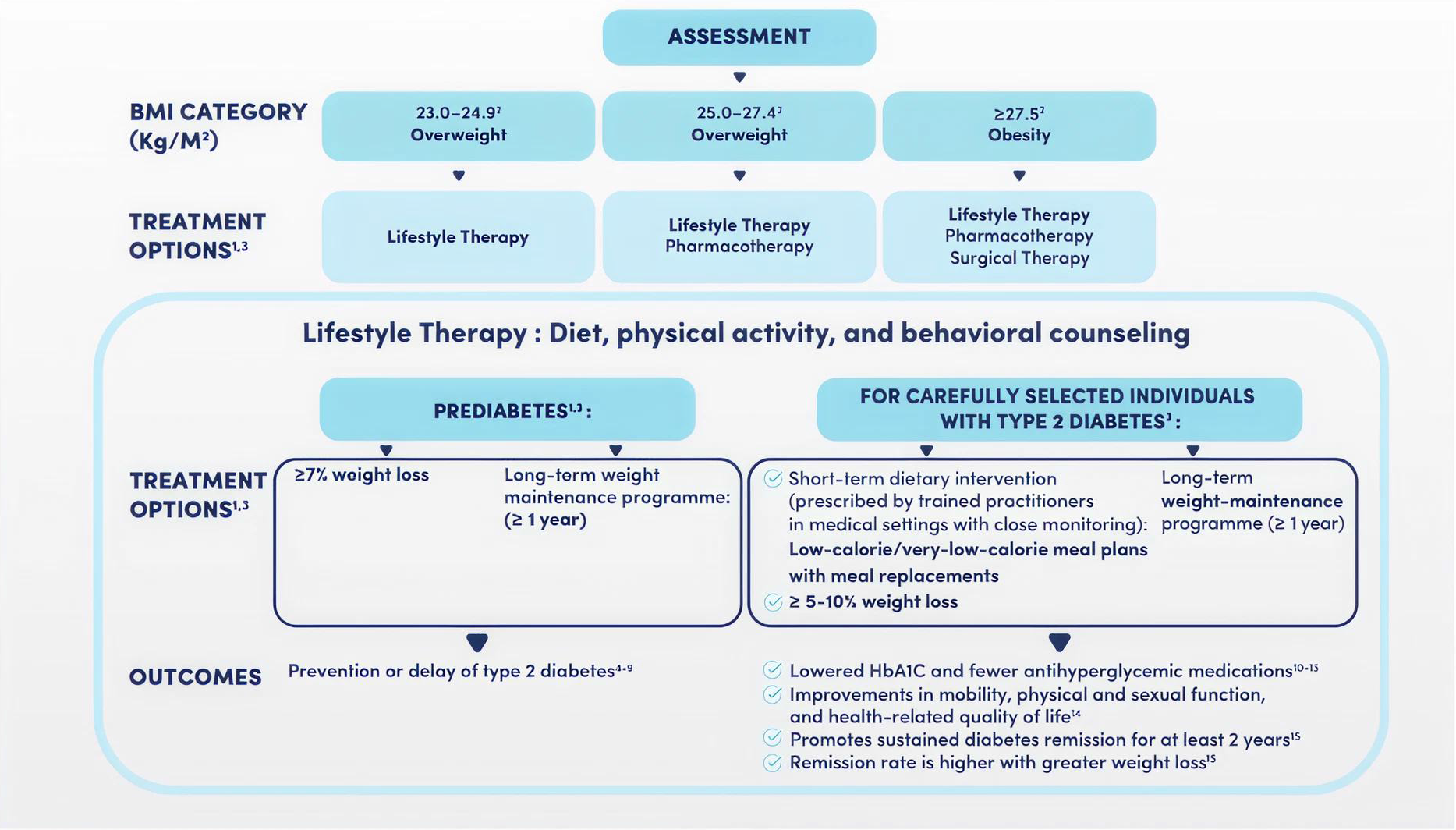
International diabetes nutrition guidelines can help healthcare professionals navigate the best dietary interventions for weight management. MRPs are aligned with most international guidelines for weight management. Figure 3 sums up therecommendationsby international guidelines for weight loss and remission of diabetes.5,10 MRPs have been found to induce greater reduction of weight compared to traditional diets.5 VLCDs, which provide 800–1,000 kcal/day, induce a substantial reduction of weight of about 14.2 kg to 21.0 kg in 11 to 14 weeks.10 Besides short-term reduction of weight, MRPs also play a critical role in maintaining lost weight.4
Summary of Guidelines on MRPs for Weight Control5-10
| Year | Organization | Guideline Statement |
|---|---|---|
| 2023 | EASO (European Association for the Study of Obesity) | In more detail, the previous guidelines stated that 'partial meal replacements (replacing one to two meals/day as part of a calorie-restricted intervention) could be used to reduce body weight, waist circumference, blood pressure and improve glycemic control,' but evidence was graded as level 1a, grade B. The addition of new evidence from literature reviews and meta-analyses indicates that meal replacements could be linked with modest to significant higher weight loss even at 1 year, may indicate a greater role of meal replacements in adult obesity.5 |
| 2022 | ANZOS (Australian and New Zealand Obesity Society) | Considerations for use as part of a low energy diet (1000–1200 kcal) where MRP substitute one or two meals, or comprehensively as part of a very low energy diet (<800 kcal/day).6 |
| 2021 | Obesity Canada | Partial meal replacements are used to replace one to two meals per day as part of a calorie-restricted intervention. These calorie-restricted interventions have been shown to reduce body weight, waist circumference, blood pressure and glycemic control compared with conventional, calorie-restricted weight loss diets. VLCDs using meal replacements include medical supervision and extensive support (nutrition, psychological, exercise counselling) as part of the intervention.7 |
| 2021 | ADA (American Diabetes Association) | Use of meal replacement plans prescribed by trained practitioners can be beneficial and the use of a partial meal replacement plan was associated with improvements in diet quality and weight loss in the Look-AHEAD trial. Structured very-low-calorie diets, typically 800–1,000 kcal/day utilizing high-protein foods and meal replacement products, may increase the pace and/or magnitude of initial weight loss and glycemic improvements compared with standard behavioral interventions.8 |
| 2016 | AACE (American Association of Clinical Endocrinology) | Meal replacements is an option for consideration when discussing meal plans as part of lifestyle therapy.9 |
| 2013 | IDF (International Diabetes Federation) | VLCD: Comprehensive, high-intensity, on-site lifestyle interventions that include a medically supervised very-low-calorie diet (often defined as <800 kcal/d), as provided by complete meal replacement products, produce total weight loss of approximately 14.2 kg to 21.0 kg over 11 to 14 weeks, which is larger than that produced by no intervention or usual care. In overweight and obese women, the use of liquid and bar meal replacements is associated with increased weight loss at up to 6 months, in comparison with a balanced deficit diet using only conventional food.9 |
Figure 3 Table Summary of Guidelines on MRPs for Weight Control5-10
Clinical Guidelines and Weight Loss Targets in T2D
Guidelines also define how much weight loss is needed to see real improvements in blood sugar levels. So, what do the latest clinical recommendations say about weight loss goals in T2D?
- For prediabetes, ≥7% of body weight loss can delay or prevent T2D.
- For T2D patients, a reduction of 5–10% body weight can reduce HbA1c, reduce drug dependency, and induce remission.2,11
Since not all patients are the same, the American Diabetes Association (ADA) provides strategies for weight management based on different BMI categories. Figure 4 illustrates a structured plan for weight management based on categories of BMI.
Figure 4 represents the ADA’s structured weight management plans based on different BMI categories:
- For all BMI categories, lifestyle therapy, which encompasses dietary change, exercise, and behavioral counseling is advised for all BMI categories.
- For a patient who is between a BMI of 25 and 27.4 kg/m², pharmacotherapy can be introduced in support of lifestyle treatments.
- For a patient who is greater than a BMI of 27.5 kg/min whom lifestyle modification and pharmacotherapy is not effective, surgical treatments can be an additional alternative.1
While global guidelines provide a broad framework, some countries have developed more detailed obesity management strategies. The Australian Algorithm for Obesity Management offers its own treatment pathways based on BMI and obesity-related complications.
The Australian Algorithm for Obesity Management
The Australian guideline for managing obesity, that is illustrated in figure 5, classifies obesity in terms of BMI and abdominal circumference. Then it recommends different strategies based on BMI categories.6
Australian algorithm for the management of obesity6
Figure 5 Australian Algorithm Treatment Based on BMI6
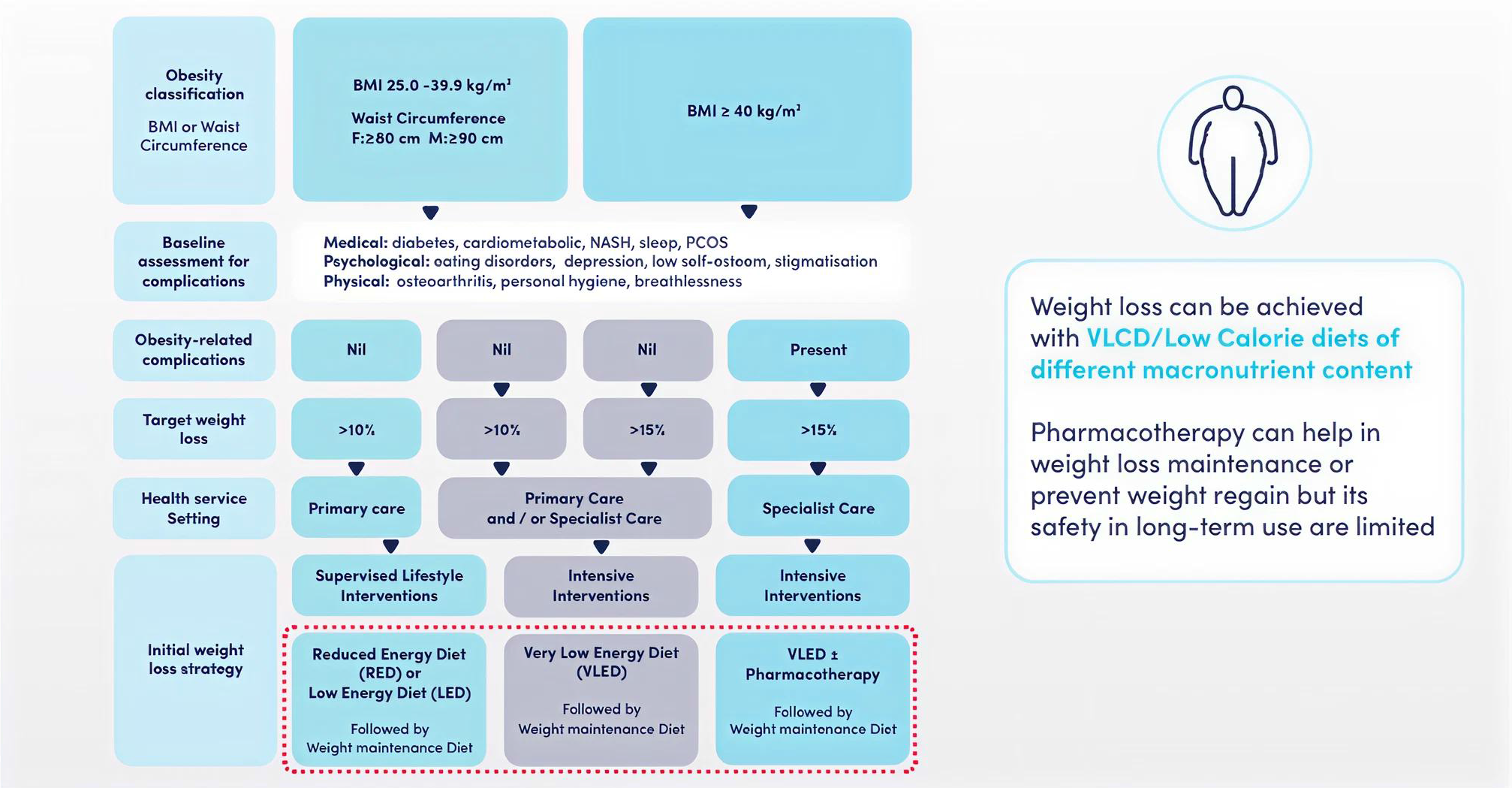
-For a patient with BMI of 25–39.9 kg/m² and a waists circumference of >80 cm for women and >90 cm for men: The Australian algorithm recommends lifestyle change, such as lower energy diets (RED) or low-energy diets (LED), followed by a plan for maintaining weight.
-For a patient of ≥40 kg/m² of BMI: The Australian algorithm recommends a very low-energy diet (VLED) along with optional drug treatment.The weight loss goal is based on complications of obesity, ranging between >10% for minimal complications and ≥15% for severe cases.6
Conclusion: Type 2 Diabetes Can Be Cured
The evidence now shows that remission of T2D is achievable through individualized weight reduction programs. Interventions such as DiRECT and DiRECT-Aus, combined with MRPs and VLCDs, provide practitioners with an evidence-based solution for managing obesity and diabetes.
What’s Next? Intensive lifestyle interventions in obesity and diabetes.
What’s Next? Intensive lifestyle interventions in obesity and diabetes.
Read HereReferences:
- American Diabetes Association. Diabetes Care. 2013;36(4):1033–46.
- American Diabetes Association. Diabetes Care. 2023;46(Suppl 1):S41–8.
- Lean ME, et al. Lancet. 2018;391(10120):541–51.
- Lean ME, et al. Lancet Diabetes Endocrinol. 2024;12(4):233–46.
- Hassapidou M, et al. Obes Facts. 2023;16(1):11–28.
- Markovic TP, et al. Obes Res Clin Pract. 2022;16(5):353–63.
- Brown J, et al. Can Adult Obes Pract Guidel. 2020; Accessed [Date]. [Note: Replace with publication details if available]
- American Diabetes Association. Diabetes Care. 2020;44(Suppl 1):S100–10.
- Garvey WT, et al. Endocr Pract. 2016;22(Suppl 3):1–203.
- Jensen MD, et al. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023.
- American Diabetes Association Professional Practice Committee. Diabetes Care. 2022;45(Suppl 1):S113–24.
Obesity is considered as one of the common triggers for the development of type 2 diabetes. As a result, a diabetes diet for weight loss that is aligned with the most updated diabetes nutrition guidelines, can help manage diabetes effectively. Learn more about the latest guideline on the most effective nutritional diabetes management.
