What is Precision Nutrition?
Precision nutrition is a new nutritional strategy that considers a person's unique attributes such as diet, phenotype, genotype, metabolic biomarkers, and gut microbiota for more targeted dietary advice. It is proposed as a new nutritional therapy approach that can be more effective in diabetes diets and in prevention of obesity. Precision nutrition aims to determine which diets work best with specific patient populations. Specifically, in diabetes care, precision nutrition intends to enhance outcomes in terms of improved glycemic control, prevention of complications, as well as increased adherence to diet.1
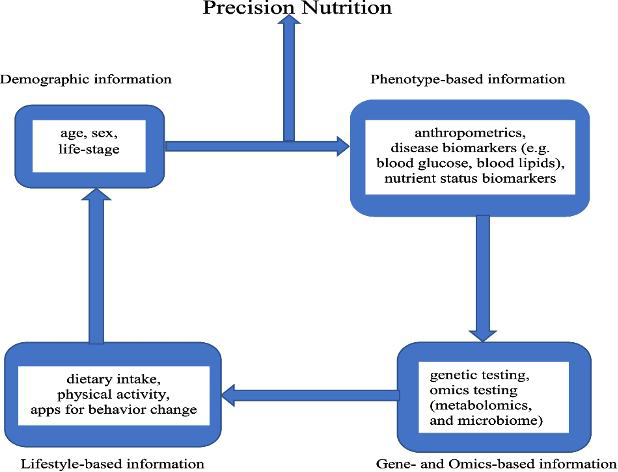
Figure 1 illustrates the precision nutrition approach. It shows how demographics, phenotype, lifestyle, genetics, and omics data are all considered. The goal is to identify variability in responses to general dietary recommendations and then optimize diets according to the detected variabilities across different groups.2
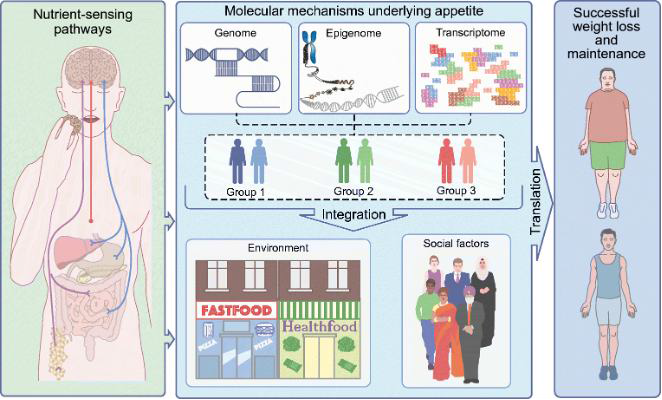
It is also noteworthy that while often used interchangeably with personalized nutrition, precision nutrition is a broader concept. It develops dietary strategies for populations based on shared molecular characteristics, whereas personalized nutrition is at the individual level. As depicted in figure 2, precision nutrition considers how individuals interact with food to improve dietary compliance. Thus, it identifies individuals with similar molecular traits (Groups 1, 2, and 3) through genetic and epigenetic profiling. Additionally, molecular data can be combined with environmental and social factors to further distinguish these groups.1
Type 2 Diabetes Diet Challenges
Dietary guidelines emphasize increasing whole foods—such as fruits, vegetables, whole grains, nuts, legumes, and seafood—while reducing refined and ultra-processed foods. However, individual responses to these recommendations vary significantly due to genetics, gut microbiota composition, lifestyle factors, and metabolic health.
The PREDICT trial highlighted this variability, showing that postprandial glucose, insulin, and fat responses to identical meals differ widely among individuals, reinforcing the need for personalized dietary strategies. Beyond variability in dietary responses, maintaining weight loss remains a major challenge. Physiological adaptations, such as lower energy expenditure and increased appetite following initial weight loss, contribute to weight regain. Additionally, behavioral factors, including difficulty adhering to long-term dietary changes, further complicate weight management. These challenges highlight the need for strategies that go beyond simple calorie restriction.1
Why Precision Nutrition in Diabetes Patients?
Diabetes is a heterogeneous disease of different etiologies and therapeutic responses. While hyperglycemia is a shared symptom, etiologies of type 2 diabetes (T2D) differ. Some T2D patients have secondary insulin resistance due to obesity; others have normal-weight insulin resistance. Historically, diabetes mellitus has been diagnosed as type 1 and type 2. With new research, there have been additional distinct subtypes recognized.1
Various Types of Diabetes
Five distinct subtypes of diabetes have been proposed based on clinical presentation:
- Severe autoimmune diabetes is type 1 diabetes or latent autoimmune diabetes in adults.
- Severe insulin-deficient diabetes is a severe form of T2D with a higher prevalence of retinopathy.
- Severe insulin-resistant diabetes is a severe form of T2D, which is marked by an increased risk of renal disease.
- Mild obesity T2D is caused by excessive adiposity.
- Mild age-related diabetes overlaps with T2D and is more common in the elderly.3
Genetic Heterogeneity in Diabetes Patients
Additional evidence of heterogeneity of diabetes is provided by genetic studies, which identify patterns of polygenic risk factors underlying metabolic dysfunctions and risk of complications. For instance, an insufficient supply of insulin due to a dysfunction of beta-cells or proinsulin production is linked with a risk of stroke. On the other hand, an insulin-resistant status which leads to obesity or liver metabolic abnormality is linked with an increased risk of coronary artery disease and liver dysfunction. Because of this variability, precision nutrition seeks to individualize therapeutic diets for patient groups, maximizing benefit. While body-weight reduction is a first-line prevention and treatment for diabetes, there is a wide variability in patient outcomes based on environmental, molecular, and social determinants.1
Evidence Supporting Precision Nutrition in Diabetes
Studies, including POUNDS LOST and PREDICT, reveal significant variability in metabolic responses to food, reinforcing the role of precision nutrition.
The POUNDS LOST RCT
This study assessed the effects of macronutrient composition on glucose metabolism based on T2D genetic risk scores. Key results included:
- Low-protein diets (15% of total energy intake) benefited individuals with lower genetic risk scores, leading to greater reductions in fasting insulin, HbA1c, and insulin resistance.
- High-fat diets (40% of total energy intake) had adverse effects in those with high genetic risk scores, increasing fasting glucose and insulin resistance.4
The PREDICT RCT
The PREDICT RCT revealed significant inter-individual variability in post-meal glucose and insulin responses following the same meals, challenging the logic of standardized diet recommendations.2
Diabetes Reversal via Digital Twin-Enabled Therapy
In a real-world observational study, precision nutrition therapy helped 82.1% of participants achieve diabetes remission within 90 days. Diabetes reversal was defined as HbA1c <6.5% at least 3 months after stopping anti-diabetic medications.5
A study in Caribbean Hispanics
The study found that the Perilipin SNP (PLIN 11482G>A) influenced obesity risk based on carbohydrate intake. Higher complex carbohydrate intake (≥144 g/day) had a protective effect against obesity. Whereas lower complex carbohydrate intake (<144 g/day) increased obesity risk.5
Tools of Precision Nutrition
Genetics, gut microbiota, and behavior all play a crucial role in shaping an individual's response to food, influencing metabolism and overall health risks.2,4
Nutrigenetics
Nutrigenetics research indicates that certain genetic risk factors are linked to higher BMI and body fat percentage, with variants in the APOA1 and APOC3 genes increasing metabolic risks, particularly in individuals consuming high-fat diets. Additionally, the PREDIMED trial found that a Mediterranean diet significantly reduced diabetes risk in individuals carrying the TCF7L2 genetic variant.2
The Gut Microbiome
The gut microbiome also affects nutrient metabolism and metabolic health. Studies show that individuals with lower Prevotella copri bacteria respond better to a Mediterranean diet, reducing heart attack risk, while specific microbes, can negatively impact blood sugar control, particularly in those consuming red meat.1
Behavior
Beyond genetics and gut health, behavior is a key factor in long-term dietary success. Findings from the Nutrigenomics Overweight/Obesity and Weight Management Trial (NOW RCT) suggest that personalized nutrition strategies enhance motivation, leading to better dietary adherence and sustainable fat reduction.2
Together, these insights highlight the need for a precision nutrition approach that integrates genetic, microbial, and behavioral factors to optimize dietary interventions.
What Does Precision Nutrition Look Like in Practice?
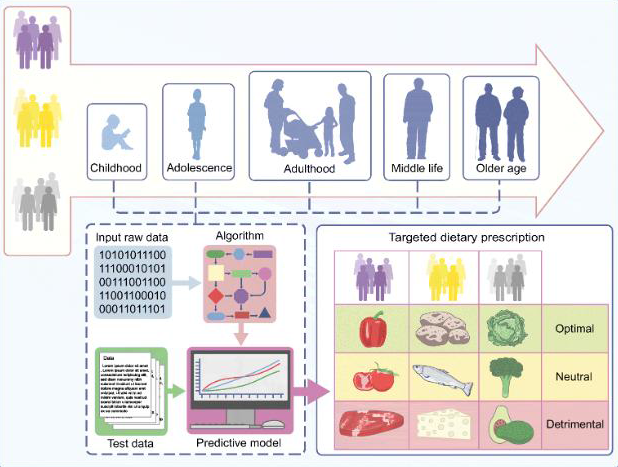
Precision nutrition combines genomics, lifestyle, and determinants of health in a patient’s diet plan. Figure 3 sums up how precision nutrition works in diabetes. The model demonstrates three hypothetical groups of individuals (purple, yellow, and grey), years before diabetes occurrence. Longitudinal, in-depth phenotypic, environmental, and social data input in a predictive engine would categorize foods as ideal, neutral, or detrimental (green, yellow, red). For instance, individuals in the purple group may benefit from peppers, and those in grey may benefit from lettuce.1
References:
- Merino J, et al. Diabetologia. 2022;65(11):1839–48.
- Antwi J, et al. Curr Nutr Rep. 2023;12(4):679–94.
- Ahlqvist E, et al. Lancet Diabetes Endocrinol. 2018;6(5):361–9.
- Huang T, et al. Am J Clin Nutr. 2016;104(1):198–204.
- Smith CE, et al. J Nutr. 2008;138(10):1852–8
Precision nutrition in diabetes diets can help healthcare professionals come up with individualized diet plans based on metabolic, genetic, and behavioral factors. Studies identify a large heterogeneity of responses to foods, which contradicts the rationale for the same dietary guidance for all patients. Learn more about this innovative approach in the nutritional management of diabetes patients.
