Diabetes Underdiagnosis
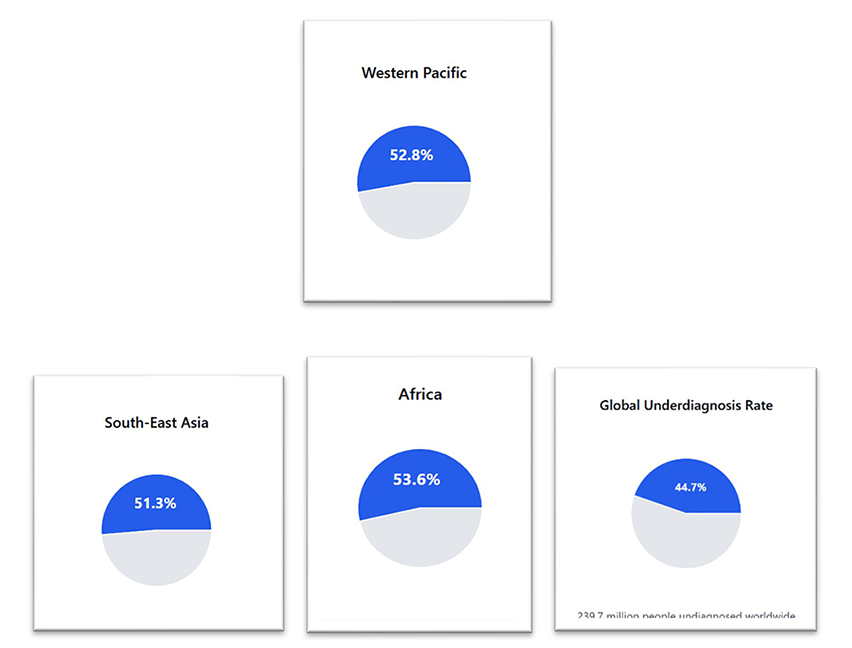
Diabetes is a growing health problem worldwide, yet a significant number of individuals remain undiagnosed and most importantly without treatment. Statistics in 2021 showed nearly half (44.7%) of all adults aged 20–79 with diabetes—approximately 239.7 million people—were undiagnosed. In Figure 1, the South-East Asia region shows one of the highest underdiagnosis rates at 51.3% and where Indonesia contributes significantly to these figures, with 14.3 million undiagnosed cases.1
The Risks of Underdiagnosis
The high prevalence rates of undiagnosed diabetes point to a serious health risk and more so as many individuals remain asymptomatic for 5–6 years. With such a delay in diagnosis, serious complications such as retinopathy, nephropathy, and coronary artery disease can arise. This is why early detection and treatment are key to prevent complications.1

How Healthcare Systems Are Tackling Underdiagnosis
With over 50% of undiagnosed cases in South-East Asia, many individuals may progress to diabetes complications.1 This is why enhancing early diagnosis is a crucial goal. Public and private health institutions and healthcare professionals are relying on different methods for early diagnosis. For example, to identify individuals at high risk of developing diabetes, targeted screening programs are used based on such WHO tools as FINRISK, ColDRISC and AUSDRISK. Other methods include digital and remote health devices, such as mobile health applications, which can enhance monitoring of individuals at risk of diabetes. While, most recently, AI predictive models can further assist in identifying individuals at risk of diabetes. All these strategies need a strong collaboration among various local and international organizations (WHO and IDF) to reach the goal of early diagnosis, early treatment and prevention of complications in type 2 diabetes1
Improving T2D treatment is also crucial for preventing complications. Multiple international guidelines recommend medical nutrition therapy (MNT) for effective management of type 2 diabetes (T2D). Among non-pharmacological MNT options, diabetes-specific formulas (DSFs) have emerged as an evidence-based therapy.8
MNT: International Guidelines
As illustrated in figure 3, various international guidelines, including the American Diabetes Association (ADA) and the International Diabetes Federation (IDF) emphasize the role of MNT in T2D:9-12
| Organization | Recommendations |
|---|---|
| ADA Standard of Care (2024)9 | An individualized medical nutrition therapy program is recommended for all people with type 1 or type 2 diabetes, prediabetes, and gestational diabetes mellitus.- Emphasize minimally processed, nutrient-dense, high-fiber sources of carbohydrate (at least 14 g fiber per 1,000 kcal).- The use of nonnutritive sweeteners as a replacement for sugar-sweetened products in moderation is acceptable if it reduces overall calorie and carbohydrate intake. |
| ADA/EASD Consensus (2018)10 | Individualized programs of medical nutrition therapy should be offered for the management of hyperglycemia. - Low-carbohydrate, low GI, high protein or Mediterranean diets may be beneficial for improving glycemic control. |
| Diabetes Canada (2018)11 | Replacing high-GI carbohydrates with low-GI carbohydrates has a clinically significant benefit for glycemic control in people with T2DM. |
| IDF (2014)12 | Diets with a low glycemic load are beneficial in improving glycemic control. - Targeting both postprandial plasma glucose and fasting plasma glucose is an important strategy for achieving optimal glycemic control. - Treating PPH can improve oxidative stress, inflammation, endothelial dysfunction, and thrombosis. - Patients with diabetes should have target HbA1c levels at <7%. |
Figure 3 - Current Management of Post-Prandial Hyperglycemia (PPH)9-12
MNT: Systematic Review and Meta-Analysis
Recent clinical trial findings further support the use of MNT for managing T2D patients. MNTs, specifically DSFs, contain higher levels of monounsaturated fatty acids (MUFAs), dietary fiber, and lower carbohydrate content.
Key findings include:
A systematic review of 19 randomized controlled trials (RCTs), 3 controlled clinical trials (CCTs), and 1 clinical trial (CT) compared DSFs with standard formulas. DSFs showed significantly lower postprandial glucose (PPH), peak glucose concentrations, and glucose AUC.13 In another meta-analysis of six RCTs, DSFs reduced postprandial glucose by 1.03 mmol/L compared to standard formulas. DSFs also showed a reduction of peak glucose concentrations by 1.6 mmol/L, a 31–45% reduction in glucose AUC and a 26–71% reduction in insulin needs.3
MNT: Goals in T2D Patients14
| Achieve and maintain body weight goals |
| Attain individualized glycemic, blood pressure, and lipid goals |
| Delay or prevent the complications of diabetes |
Figure 4 - 2024 Goals of Nutrition Therapy for All People with Diabetes14
Conclusion
Early diagnosis and early treatment initiation are essential in diabetes management for both glycemia control and prevention of long-term complications. MNT in the form of DSFs has shown evidence as an impactful non-pharmacological therapy in T2D patient care.
References
- Ogurtsova K, et al. Diabetes Res Clin Pract. 2022;183:109118.
- Fong DS, et al. Diabetes Care. 2003;26(Suppl 1):S99–102.
- Hypertension in Diabetes Study Group. J Hypertens. 1993;11:309–17.
- Molitch ME, et al. Diabetes Care. 2003;26(Suppl 1):S94–8.
- Kannel WB, et al. Am Heart J. 1990;120:627–76.
- Gray RP, Yudkin JS. Textb Diabetes. 2nd ed. Blackwell Sciences; 1997.
- King’s Fund. Counting the cost. London: British Diabetic Association; 1996.
- Mayfield JA, et al. Diabetes Care. 2003;26(Suppl 1):S78–9.
- American Diabetes Association. Diabetes Care. 2024;47(Suppl 1):S1–4.
- Davies MJ, et al. Diabetes Care. 2018;41:2669–701.
- Diabetes Canada CPG Expert Committee. Can J Diabetes. 2018;42(Suppl 1):S1–325.
- Int Diabetes Fed Guideline Dev Group. Diabetes Res Clin Pract. 2014;103:256–68.
- Elia M, et al. Diabetes Care. 2005;28:2267–79.
- Diabetes Care. 2023;46(Suppl 1):S68–96.
Based on the International Diabetes Federation (IDF) statistics, nearly half of all adults with diabetes worldwide remain undiagnosed. This is equivalent to around 239.7 million people unaware of their condition. Particularly in South-East Asia undiagnosed diabetes rates exceed 50%. Learn more about solutions for this problem and how diabetes-specific formulas can help your patients control their blood glucose.
