Diabetes-Specific Nutrition
Food for a diabetes diet can include meal replacements in the form of oral nutritional supplements (ONS) for weight management and post-meal blood glucose control. In practice, ONS have been extensively prescribed in medical nutrition therapy. Recently, clinical studies comparing standard ONS vs. diabetes-specific ONS (DS-ONS) have all confirmed DS-ONS are superior for T2D patients. The science behind this special diabetes food is based on a balance of macronutrients designed to meet the needs of patients with diabetes. Specifically, DS-ONS formulations have been developed with more proteins, less carbohydrates, and more fiber. This article provides a summary of clinical studies that demonstrate the evidence-based outcomes of DS-ONS in diabetes patients.1-4
Clinical Trials Supporting Special Diabetes Food
Scientific evidence is continuously in favor of special diabetes food such as the DS-ONS in controlling glycemia in T2D patients. DS-ONS have shown superiority compared to normal ONS and usual meals. How can DS-ONS help T2D patients? DS-ONS better reduce postprandial glucose levels, enhance sensitivity to insulin, and enhance metabolic status in the long term. The following is a review of key clinical study results on DS-ONS.1-4
1- Klosterbuer A, et al. Study
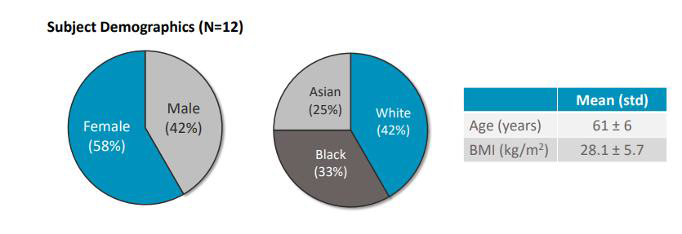
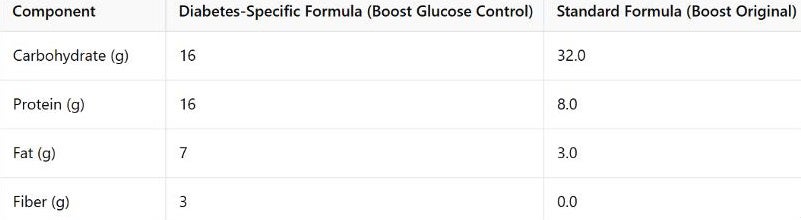
This was a randomized crossover trial involving 12 participants. The aim was to compare DS-ONS (BOOST Glucose Control) with a standard ONS.1 The demographics of participants and the nutritional composition of both formulas in this study are illustrated in figures 1 and 2:
| Nutritional Composition (Per Serving) | DS-ONS | Standard ONS (Control) |
|---|---|---|
| Protein g (%Total Energy) | 16g (33% TE) | 7.9g (17% TE) |
| Fat | 7g (33% TE) | 3.2g (15% TE) |
| Carbohydrates | 16g (34% TE) | 32g (68% TE) |
| Fiber | 3g | 0g |
Figure 2 nutritional composition of the two formulas used in the klosterbuer study
(TE = Total Energy)
Klosterbuer et al. Key Findings:
- DS-ONS significantly reduced glucose area under the curve (AUC) and peak glucose (Cmax) compared to the standard ONS (p < 0.01).
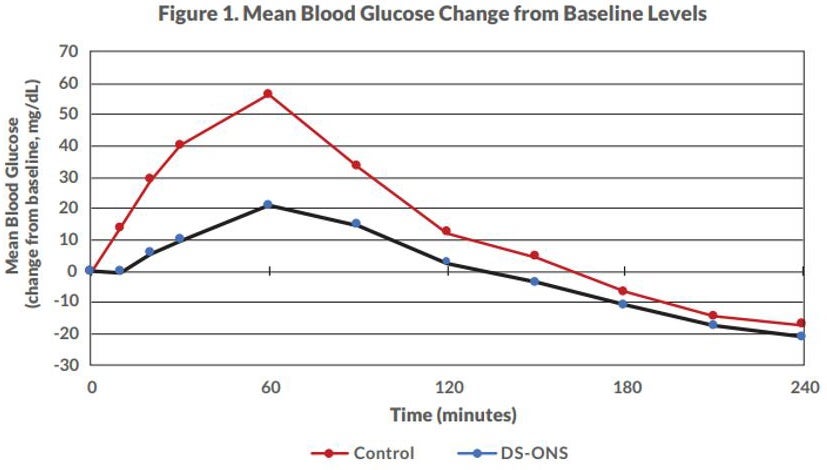
Figure 3 shows mean blood glucose AUC and Cmax for blood glucose were significantly lower for DS-ONS vs. Control (p<0.01). Note: The original study included separate comparisons of two DS-ONS formulations vs. control. As one formulation is no longer commercially available, this summary was simplified to include only the existing DS-ONS
- While insulin Cmax was lower for DS-ONS, overall insulin AUC showed no significant differences.
In sum, the Klosterbuer A, et al. study confirms that DS-ONS can help reduce blood sugar spikes and improve glycemic control in T2DM patients, supporting their integration into clinical care.1
- Huhmann MB, et al. Study
In this study, Huhmann et al. investigated the role of a diabetes-specific ONS (BOOST Glucose Control) vs. a standard ONS (BOOST Original) in a randomized crossover trial:
Study Demographics of participants in the Huhmann MB et al. study are presented in the following table:
| Participant Demographics | Mean ± SD |
|---|---|
| Age | 59.5 ± 9.6 years |
| BMI | 31 ± 5 kg/m² |
| Gender | 7 men (58%), 5 women (42%) |
| Baseline HbA1c | <9.0% |
| Baseline FPG | <180 mg/dL |
| Comorbidities | Hypertension (58%), Hyperlipidemia (50%), Fatty Liver Disease (17%) |
| Medication Use | Metformin (83%), Antihyperlipidemic drugs (50%), Antihypertensive drugs (58%) |
Figure 4 Participants' demographics in huhmann MB et al. study
2- Huhmann et al. Key Findings:
- The DS-ONS significantly lowered glucose AUC compared to the standard ONS.
The mean glucose AUC was significantly lower in the DS-ONS group compared with standard ONS (p<0.0001).
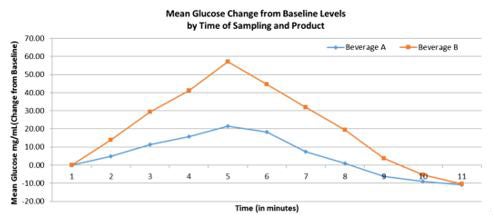
Figure 6 shows mean glucose change from baseline by treatment product (standard ONS and diabetes-specific ONS).
- As for insulin, a sensitivity analysis revealed that insulin AUC was significantly lower for DS-ONS after removing an outlier.
There was no significant difference observed for mean insulin AUC (p=0.068). A sensitivity analysis of the mean insulin AUC measures was performed to identify any potential outliers. One outlier was identified, which was observed to have an insulin AUC value more than twice as high as the next highest value. Thus, this value was removed from analyses, resulting in a significant difference between the groups (p=0.012).
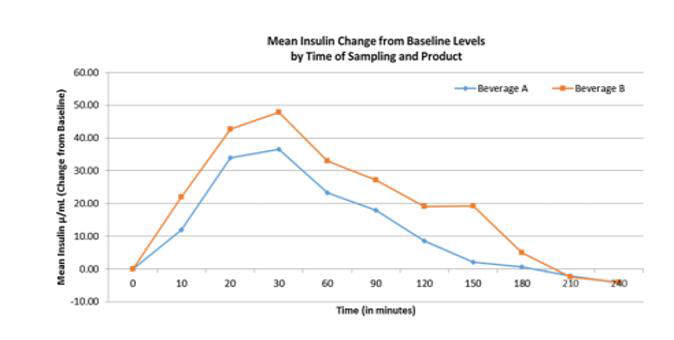
Figure 7 Mean insulin change from baseline by treatment product (standard ons vs diabetes-specific ons)
In conclusion, the Huhmann MB, et al. study findings further support the use of DS-ONS for stabilizing postprandial glucose levels and reducing glycemic variability in T2D patients.
3- Gulati et al. Study
In this study, Gulati et al. compared a DS-ONS (NUTREN Diabetes) with an isocaloric meal of cornflakes and milk in a randomized crossover trial.3
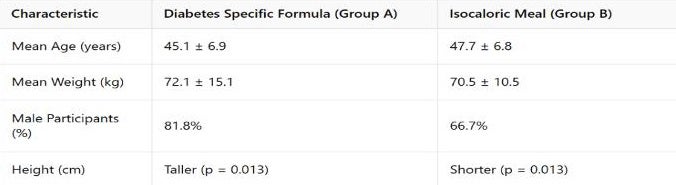
Demographics
The study enrolled a total of 40 participants with T2DM, divided into two groups. Baseline characteristics, such as weight and HbA1c levels, were similar between both groups.
| Macronutrient Composition of NUTREN Diabetes | % of Total Energy Intake (TEI) |
|---|---|
| Protein | 15% |
| - Whey Protein | 50% |
| - Casein Protein | 50% |
| Carbohydrates | 45% |
| Total Fats | 40% |
| Fiber | 15.3g per 1000 kcal |
| Glycemic Index (GI) | 22 (below recommended ≤55 for diabetes) |
Gulati et al. Key Findings
- The formula significantly reduced post-meal glucose levels at 30, 60, 120, and 180 minutes3.
Figure 10 shows the AUC for blood glucose post-meal at 30 min, 60 min, 120 min, and 180 min was significantly lower for Group A as compared with Group B (p = 0.003, 0.0001, 0.0001, and 0.0001, respectively).
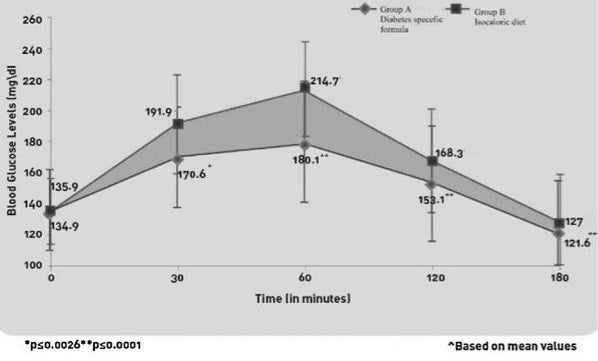
Figure 10 Area under curve (auc) for blood glucose in group a and group b - As for insulin, serum insulin levels were notably lower at 120 and 180 minutes3.
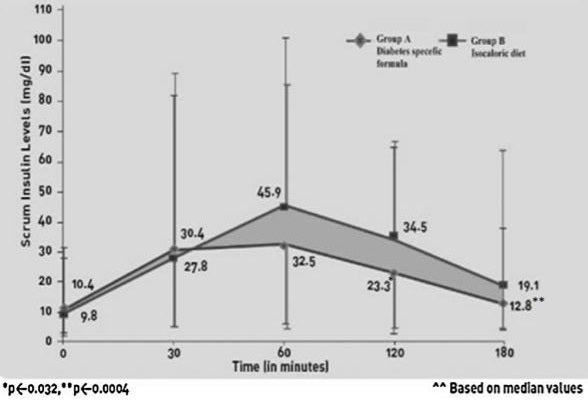
Figure 11 shows the AUC for serum insulin was significantly lower for Group A post-meal at 120 min and 180 min (p value at 30 min = 0.2111, at 60 min = 0.1087, at 120 min = 0.0002, and at 180 min = 0.0007). Mean serum insulin levels for both the groups are presented.
Figure 11 area under curve (AUC) for serum insulin in group a and ggroup b
In sum, the Gulati et al. study findings reinforce the role of DS-ONS in achieving better glycemic control as an effective approach to controlling postprandial hyperglycemia, further substantiating their use in medical nutrition therapy.
4-The Phanachet et al. Study: “The Efficacy and Safety of NUTREN Diabetes: A Randomized Study in Patients with Type 2 Diabetes Mellitus”4
This was a randomized, open-label, crossover study conducted at Ramathibodi Hospital, Mahidol University, Thailand. Thirty patients with T2D participated in the study, receiving either a DS-ONS NUTREN Diabetes (Group A) or a standard isocaloric diet (Group B) in the first phase. After a one-week washout period, the groups switched interventions.4
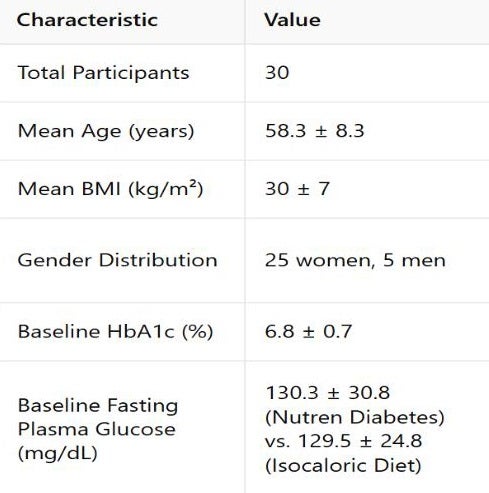
Composition of the test meal and the diabetes-specific formula (DSF) in the Phanachet et al. study4
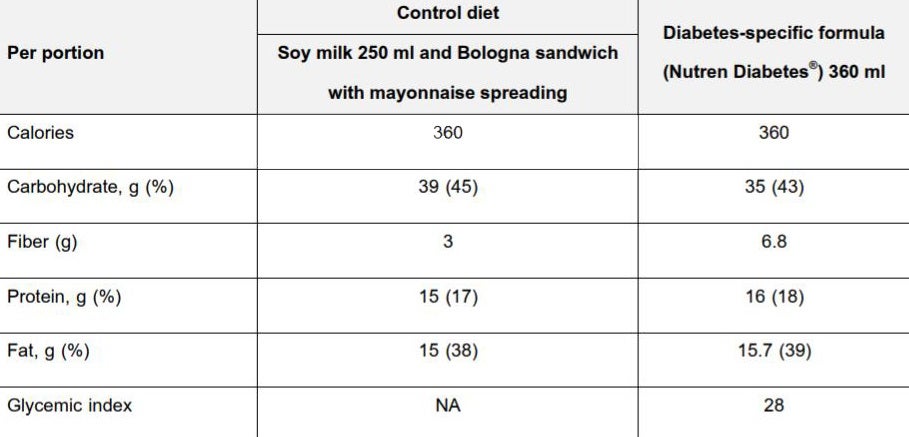
Phanachet et al. study Key Findings
1- Postprandial hyperglycemia (PPH) levels in the DS-ONS (NUTREN Diabetes) group were significantly lower than those in the isocaloric diet group at 120 minutes (161.4 ± 37.9 mg/dL vs. 197.7 ± 56.8 mg/dL; P=0.005)4
The incremental area under the curve (iAUC) for glucose was significantly lower for DS-ONS (NUTREN Diabetes) compared to the standard diet (4,859.5 vs. 6,551.7; P=0.007)4
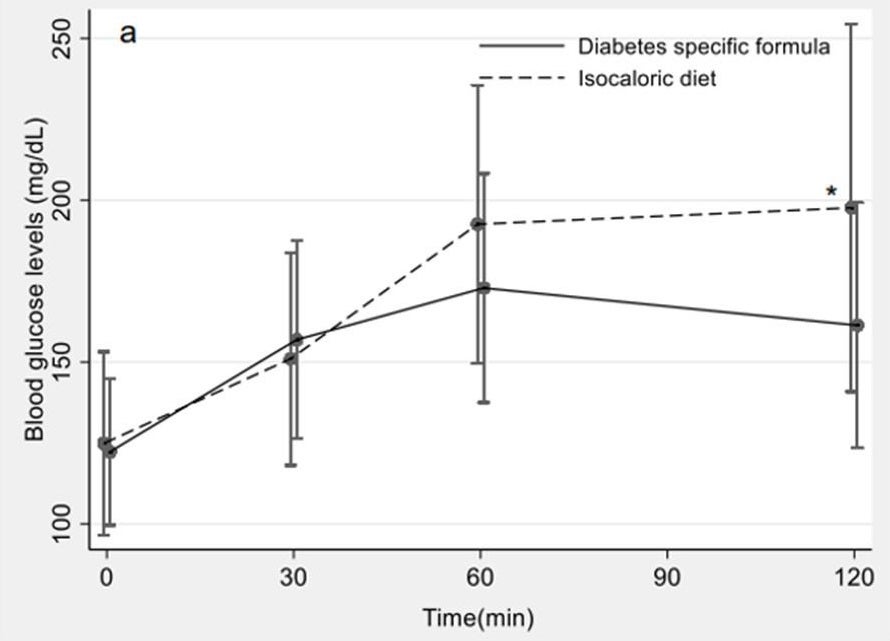
- As for insulin levels, postprandial insulin levels were lower at 60 and 120 minutes in the DS-ONS (NUTREN Diabetes) group, however, the differences were not statistically significant.
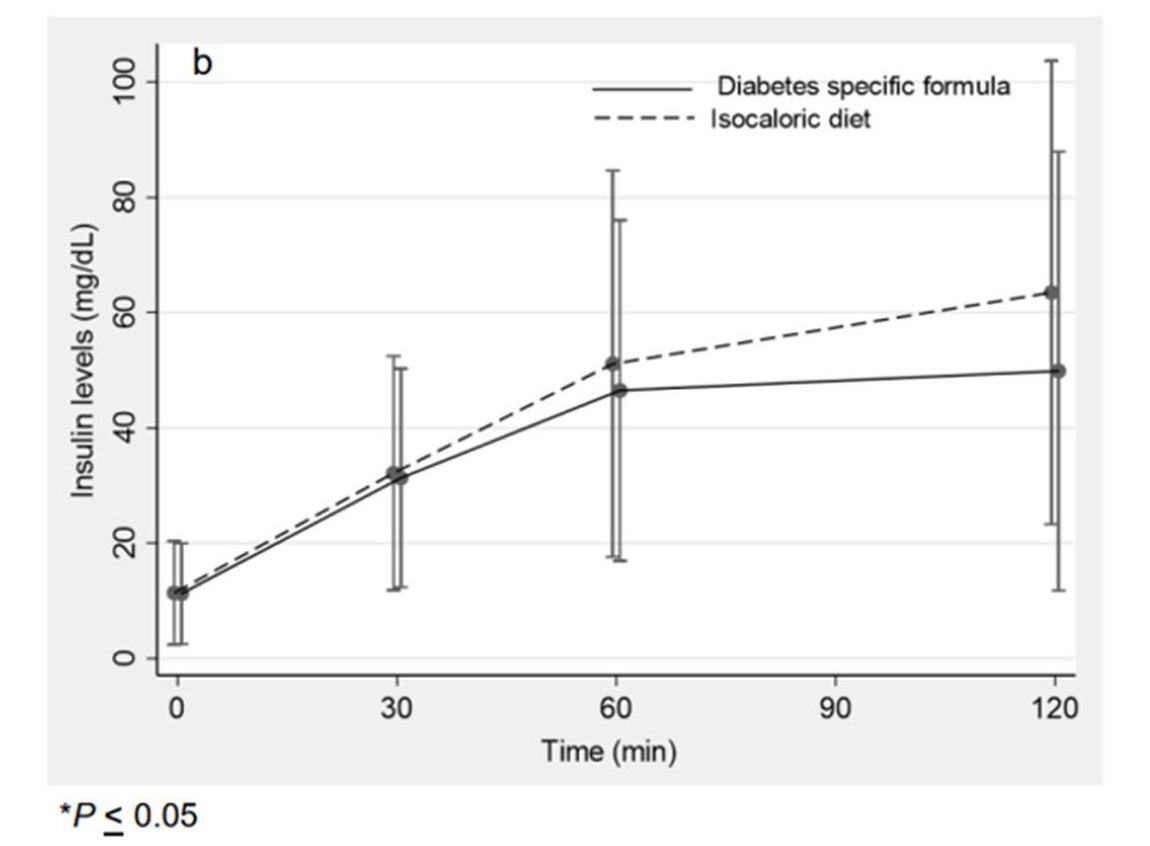
Figure 15 shows the 2-hour postprandial insulin level graph in DSF and isocaloric diet in the phanachet et al. study
Diabetes Diet Foods: Final Thoughts
All the outcomes of these large clinical trials affirm DS-ONS as an evidence-based medical nutrition therapy in T2D care. By lowering postprandial glucose levels, reducing glycemic variability, and preserving metabolic health, DS-ONS represent a practical nutritional solution for t2D patients. DS-ONS, unlike standard ONS, comprise lower glycemic index complex carbohydrates, more protein, and more micronutrients to meet the needs of diabetes patients.1-4
References:
- Klosterbuer A, et al. JPEN J Parenter Enteral Nutr. 2021;45(Suppl 1):S194–5.
- Huhmann MB, et al. Diabetes Res Clin Pract. 2016;115(Suppl):35–41.
- Gulati S, et al. Diabetes Metab Syndr. 2015;9(3):192–7.
- Phanachet P, et al. J Nutr Thailand. 2021;56(1):1–10.
This article presents the science behind special diabetes food. Diabetes-specific oral nutrition supplements, which consist of a tailored macronutrient composition have proven efficacy for glycemic control. Discover an overview of posters and publications of large clinical trials comparing DS-ONS vs. standard ONS in type 2 diabetes patients. Evidenced-based outcomes support integration of DS-ONS in medical nutrition care for diabetes patients.