Breakfast Nutrient Composition for Diabetes
The macronutrient content in breakfast is an important decision in a diabetes meal plan. In the past decades, low-fat meals were recommended for reducing cardiovascular risk, a frequent comorbidity of type 2 diabetes (T2D), by lowering cholesterol levels. In doing so, however, these low-fat meals usually resulted in fat being replaced by carbohydrates, in large part in the forms of cereals and sugar, which have led to glycemic instability.1 In contrast, studies confirm that a diabetes low carb diet, high-protein breakfasts result in better glycemic control, insulin action, and release of incretins.2,3 This article delves into the science of breakfast ingredients for managing diabetes.
Why Nutrient Composition Matters?
Breakfast content is important for metabolic well-being, in particular for managing blood sugar. High-carbohydrate, low-fat meals induce spikes and subsequent crashes in glucose.1 In contrast, high-protein, low-carb diets for breakfast result in greater satiety and improved glycemic control throughout the day.2
Low Carb Diet for Diabetes: A Clinical Study
To assess the role of breakfast composition in T2D clinically, a randomized controlled trial was conducted by Oliveira et al. The study compared results of Low-Carbohydrate (LC) vs. a Low-Fat Breakfast (CTL) in T2D over 12-week cycles. The study randomly assigned patients to either of two regimes
- LC Breakfast: 465 kcal, 8g carbohydrates, 25g proteins, 37g fat
- CTL Breakfast: 450 kcal, 56g carbohydrates, 20g proteins, 15g fat2
Highlights of Key Findings from the Oliveira et al. Study
Improved Glycemic Control:
This study showed enhanced glycemic control in individuals who ate LC breakfasts in relation to those who ate CTL breakfasts. There was a greater reduction in hemoglobin A1C (HbA1c) in the LC group (-0.3% vs. -0.1%, p=0.06). The mean glucose in the LC group was lower by −0.7 mmol/L (95% CI: −1.4, −0.1 mmol/L, P=0.03), while no change in the CTL group.
Maximum glucose levels in group LC went down (-1.3 mmol/L, 95% CI: -2.3, -0.4 mmol/L, P=0.01), a substantial drop compared with the CTL group.
Glycemic variability, quantified using MAGE, was lower in LC group (-0.8 mmol/L, 95% CI: -1.2, -0.3 mmol/L, P < 0.01), which means better blood glucose stability. The LC breakfast participants spent 77% more time in the ideal glucose range of 3.9–10 mmol/L than participants in the CTL group.2
Better postprandial glucose regulation:
The LC meal suppressed postprandial glycemic spikes, evidenced by a lower glucose incremental area under the curve (iAUC).2
Enhanced Hormonal and Metabolic Responses:
The postprandial glucose levels in the LC group were maintained due to rising GLP-1 levels, and appetite signals were suppressed.2
Enhanced Dietary Adherence:
The LC group members exhibited greater compliance with the meal plan. The LC group had lower carbohydrate intake (-73 g; 95% CI: -101, -44 g; P < 0.01) and lower caloric intake (-242 kcal; 95% CI: -460, -24 kcal; P = 0.03).2
High-Protein Breakfasts
Protein is a key macronutrient in breakfast for controlling diabetes. Protein has unique metabolic actions which translates into a better endocrine reaction, satiety, and blood glucose levels.3,4
Comparing High-Protein vs. High-Carbohydrate Breakfast in T2D
A paper by Park et al. differentiates between the effect of a high-protein compared to a high-carbohydrate breakfast on glucose, insulin and incretin hormones, over eight hours. The study also looked at the potential of a high-protein breakfast in preparing the body for improved glycemic control in subsequent meals, the so-called “second-meal effect”.3
Park et al. Study Design
The study consisted of 12 T2D individuals who ate breakfast every day. Participants consumed either breakfast for six days:
A High-Protein Breakfast (PRO): 500 kcal, 35% Protein, 45% carbohydrate, 20% fat
or
A carbohydrate-rich breakfast (CHO): 500 kcal, 15 g of proteins, 65 g of carbohydrate, 20% fat
On the seventh day, after an overnight fasting, study participants consumed a designated breakfast and, four hours subsequently, a standard meal of high carbohydrate content.3
Key Findings from the Park et al. Study
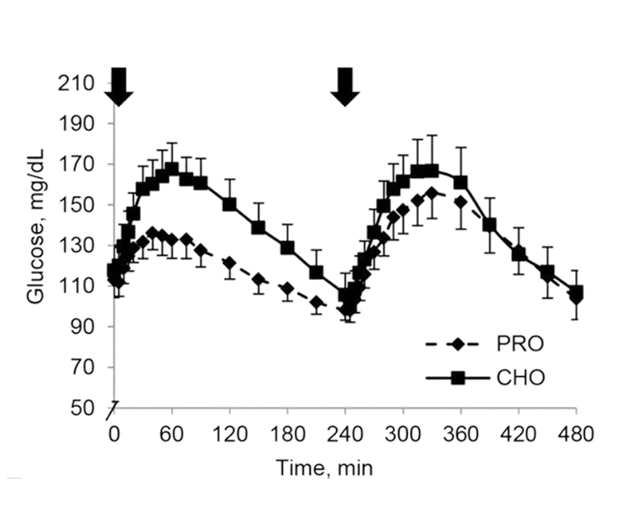
The post-meal glucose area under curve (AUC) levels in the PRO meal were 16% lower than in the CHO meal. Figure 1 shows Glucose AUC in the PRO group compared to the CHO group followed by a normal lunch that is the same for both groups of T2D patients.3
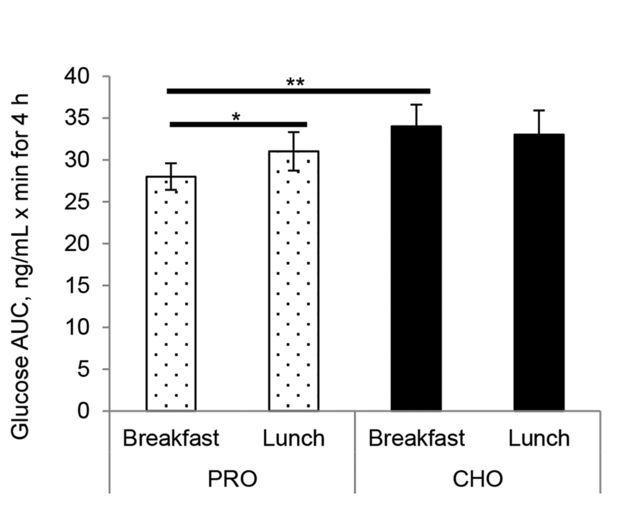
followed by the same lunch for both groups.3
Post-Breakfast Insulin Response:
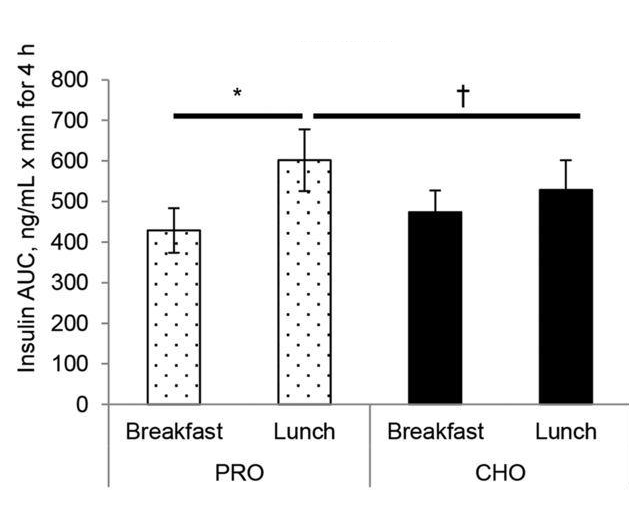
Although peak insulin levels were lower with the PRO breakfast, insulin AUCs remained comparable between the two. However, the PRO breakfast primed β-cells for a robust insulin response during the subsequent meal, known as the "second-meal phenomenon" described later in this article.
Figure 2 shows Insulin AUC responses to either a PRO or a CHO breakfast and a standardized lunch in T2D.3
Incretin Hormones (GLP-1 and GIP):
GLP-1 secretion was 27% higher after the PRO breakfast compared to the CHO breakfast. This sustained GLP-1 release contributed to improved glycemic control and reduced glucose variability. Figure 3 shows GLP-1 AUC responses to either a PRO or a CHO breakfast and a standardized lunch in T2D.3
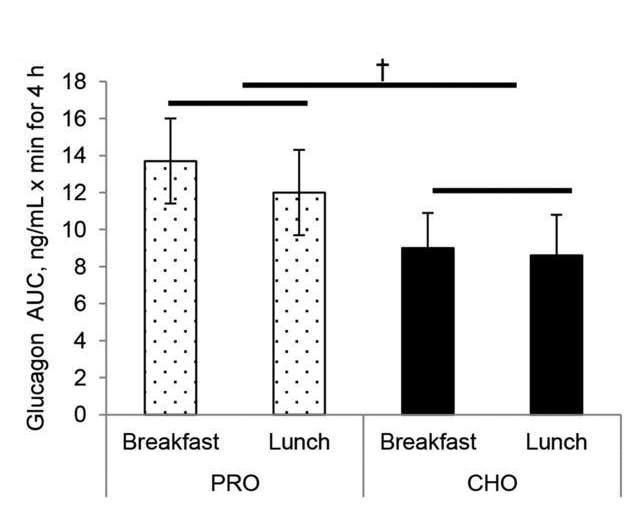
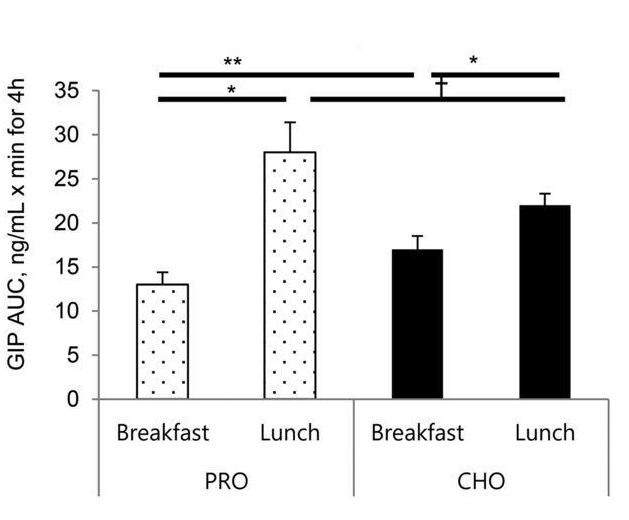
GIP levels were higher during the post-lunch period, indicating a primed incretin response that facilitated better glycemic control even at the subsequent meal. Figure 4 below shows GIP AUC responses to either a PRO or CHO breakfast and a standardized lunch in T2D.3
Second-Meal Phenomenon
The high-protein breakfast enhanced the second-meal insulin response, which helped mitigate postprandial glucose spikes following lunch. Figure 5 illustrates how a high-protein breakfast helps maintain better glycemic control throughout the day, as shown by the reduced blood glucose fluctuations (green line) compared to a carbohydrate-rich breakfast (gray line). This supports the "second-meal phenomenon," where protein intake at breakfast improves blood sugar responses to subsequent meals.3
A high protein breakfast can lead to greater glycemic control:
Protein Source Matters
The source of proteins determines the degree of benefit for blood glucose levels. Of all proteins, whey is ideal owing to its rapid absorption, rich BCAA content, and ability for inducing release of insulin and GLP-1. In comparison with other proteins such as casein, egg, and soy, whey is superior in T2D care.4
Conclusion
Breakfast for diabetes diets can help control diabetes. Protein-rich, carbohydrate-low meals for breakfast have major benefits, including lower post-meal glucose levels, enhanced glycemic variability, and enhanced GLP-1 hormonal release. Small meal composition changes can make a big difference in aiding patients with diabetes.
Learn more about The Science Behind Special Diabetes Food.
Read HereReferences:
- Ludwig DS, et al. Am J Clin Nutr. 2023;118:849–51.
- Oliveira BF, et al. Am J Clin Nutr. 2023;118:209–17.
- Park YM, et al. J Nutr. 2015;145:452–8.
- Jakubowicz D, et al. J Nutr Biochem. 2017;49:1–7.
Breakfast Nutrient Composition for Diabetes The macronutrient content in breakfast is an important decision in a diabetes meal plan. In the past decades, low-fat meals were recommended for reducing cardiovascular risk, a frequent comorbidity of type 2 diabetes (T2D), by lowering cholesterol levels. In doing so, however, these low-fat meals usually resulted in fat being replaced by carbohydrates, in large part in the forms of cereals and sugar, which have led to glycemic instability.1 In contrast, studies confirm that a diabetes low carb diet, high-protein breakfasts result in better glycemic control, insulin action, and release of incretins.2,3 This article delves into the science of breakfast ingredients for managing diabetes.